The Biology of Periods
The Biology of Periods by Dr Dawn Harper
Dr Dawn Harper is a GP and leading media medic.
Do you know your corpus luteum from your pituitary gland?
Incredibly, 1 in 5 women – and over a third of men – don’t know where period blood comes from, with some thinking it comes from the bladder![1] If we don’t understand the basics of the menstrual cycle, then how are we to know what’s normal and what’s not, when it comes to periods? The following article will help bring to life the biology of a period.
During the menstrual cycle, the wall of the uterus thickens with tissue and an egg is released from the ovary. If the egg is not fertilised, the body will shed the tissue through the vagina. The menstrual cycle is controlled by hormones and occurs in four phases; menstruation, follicular phase, ovulation, and luteal phase (see image below).
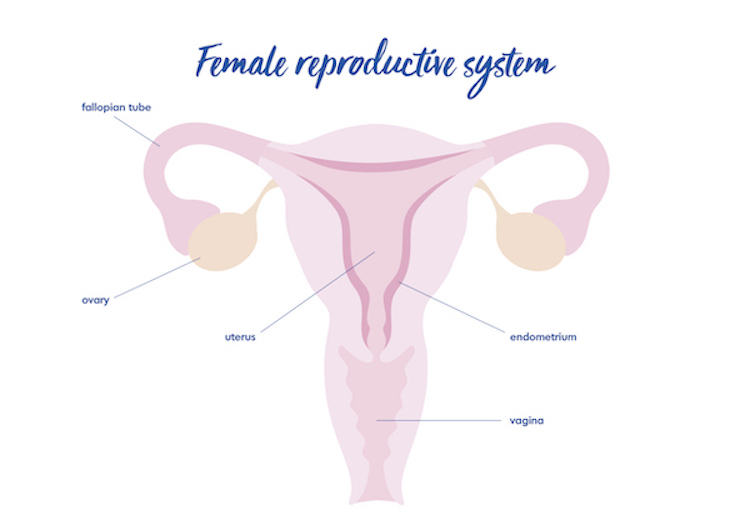
Menstruation: menstruation is when the thickened lining of the uterus (endometrium) leaves the body through the vagina. The lining of the uterus supplies a fertilised egg with nutrients, so if the egg isn’t fertilised, then the lining is no longer needed.
Follicular phase: beginning on the first day of menstruation, the pituitary gland (a hormone-releasing gland located at the base of the brain) releases follicle-stimulating hormones (FSH). These hormones cause follicles to develop in the ovaries, which bead on the surface and eventually, one will burst to release an egg. These follicles also cause a rise in oestrogen levels, causing the uterus lining to thicken.
Ovulation: the rise in oestrogen causes the levels of FSH and the luteinising hormone (LH) to increase. This occurs mid-way through the cycle and triggers the egg to be released into the uterus for fertilisation.
Luteal phase: the follicle where the egg originated remains on the surface of the ovaries and forms a structure called corpus luteum, releasing the hormones progesterone and oestrogen. This maintains the thickened lining of the uterus for a fertilised egg to attach. But, if the egg remains unfertilised, it will die along with the corpus luteum. The lining of the uterus is then expelled from the body, and the cycle repeats.
On average, menstrual cycles last between 21-35 days. Your period can last between 2 and 7 days, but it will usually last for about 5 days[2]. If you are bleeding for more than seven days and your period occurs more frequently, then you could be suffering from heavy periods[3].
Heavy bleeding, formally known as menorrhagia, is a medical condition. This is a treatable condition, with several treatment options available. This includes hormonal and non-hormonal treatments, as well as surgeries such as endometrial ablation, fibroid and polyp removal, and a hysterectomy. Research shows that nearly 1 in 2[4,5] women suffer from heavy periods so there’s absolutely nothing to be embarrassed about.
Find out more about visiting your GP to talk about heavy periods and to take back control of your menstrual cycle. Heavy bleeding can have a big impact on both physical and mental health, so it’s important to get checked out.
Wear White Again is a Hologic campaign.
References
[1] – Data on file: MISC-05658-GBR-EN Rev 001
[2] – NHS (2019). Overview – Periods. [online] NHS. Available at: https://www.nhs.uk/conditions/periods/. [last access: 26/06/2023]
[3] – Royal College of Obstetricians and Gynaecologists. National Heavy Menstrual Bleeding Audit (May 2011). Last accessed July 2019, available https://www.rcog.org.uk/globalassets/documents/guidelines/researchaudit/nationalhmbaudit_1stannualreport_may2011.pdf
[4] – Data on file: MISC-08708-GBR-EN Rev 002
[5] – Survey of 2,000 Women aged 18-55 plus top up 1,000 UK women who have heavy menstrual bleeding during October 20th – 27th 2022. MISC-08708-GBR-EN [last access: 26/06/2023]